Highlights
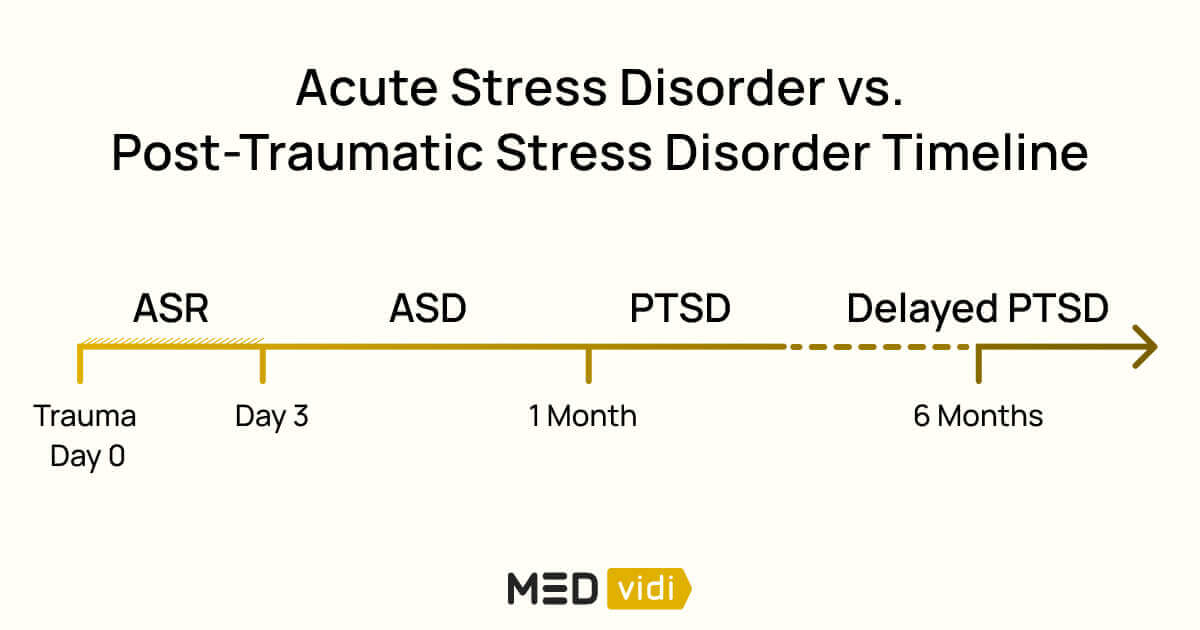
- An acute stress reaction, or the fight-or-flight response, is triggered by an immediate threat or challenge; it results from adrenaline release and is usually short-lived.
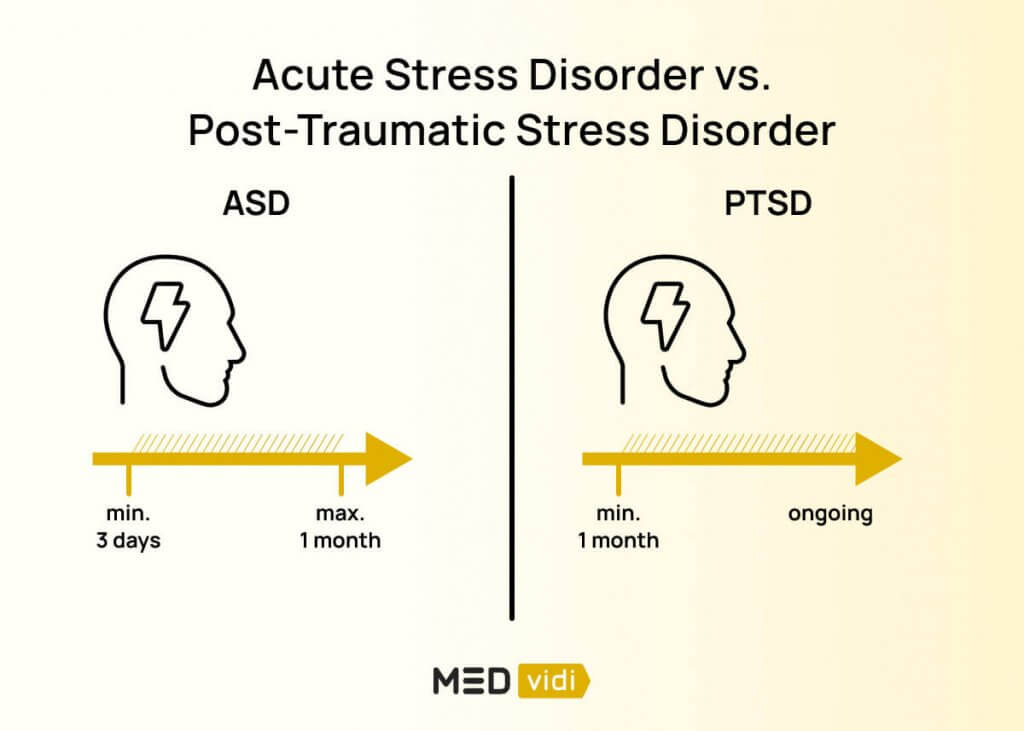
- Acute stress disorder
refers to a severe stress reaction[1] lasting between 3 days and 4 weeks following a trauma exposure. - Post-traumatic stress disorder is a long-term mental health condition, with symptoms present for more than a month, triggered by a traumatic event, and it lasts for months or years.
- The primary difference between acute stress disorder and post-traumatic stress disorder is in the timeline, with the cut-off and transition at one month; however, many of their triggers, risks, symptoms, and some treatment options overlap.
Many people might have heard the term PTSD, post-traumatic stress disorder, but don’t know much about it. In this article, we’ll look at trauma and stressor-related disorders in more detail, highlighting two: acute stress disorder (ASD) vs PTSD.
This is an essential topic because trauma can happen to anyone; worryingly, a World Health Organization survey found that
It is also essential to know the difference between ASD and PTSD when choosing appropriate treatment and for implementing prevention strategies.
But before we get into the details, you need to understand that the starting point for both ASD and PTSD is an acute stress reaction.
Acute Stress Reaction (ASR) and Traumatic Stress Reaction Explained
An acute stress reaction, which you may know as the fight-or-flight response,
Aside from fight and flight, other ASR responses include
A traumatic stress reaction, on the other hand, is an acute stress reaction triggered by a traumatic event.
Trauma is different from stress
Trauma occurs when an event is experienced as physically or emotionally harmful and has lasting mental and emotional distress, as well as possible physical, social, or spiritual effects.
So, a traumatic stress response is more severe and lasts longer than an acute stress response.
But why do some people recover within hours or days, and others battle for months or years? It is related to something called
Let’s illustrate this with two examples:
- Someone who has a serious car wreck may have ASR symptoms every time they drive or if they hear the song that was on the radio at the time of the accident.
- A person who was mugged outside a restaurant after dinner with friends might experience a fight-or-flight response after dark or even with an invitation to an evening get-together.
Now, let’s take a closer look at ASD and PTSD.
What Is Acute Stress Disorder (ASD)?
Acute stress disorder (ASD) is an ‘extended’, but still relatively short-term reaction to a traumatic event that causes mood, thought, and behavior changes
Unfortunately, there are
- Motor vehicle accident — 13 to 21%
- Traumatic injury — 44%
- Assault — 16 to 19%
- Burns — 10 %
- Witnessing a mass shooting — 33%
The possible symptoms for ASD
- Dissociative Symptoms. These
often occur in ASD[7] ; what does this mean exactly? People might feel detached from their bodies and emotions, like they’re watching themselves from the outside, floating about, or like their body doesn’t feel real. Also, they may not remember details of the trauma because their brain protects them by blocking the memory. - Arousal Symptoms. These include issues with sleep, reckless or self-destructive behavior, irritable or aggressive outbursts, being always alert to danger, difficulty concentrating, and an extreme startle response.
- Intrusion Symptoms. Having recurrent, involuntary, and intrusive thoughts; people might experience distressing nightmares, flashbacks, or have physical reactions or emotional distress when exposed to traumatic reminders.
- Avoidance Symptoms. Avoiding thoughts and feelings about the event, becoming numb; avoiding people, places, and situations that remind them of the trauma.
- Negative Mood. People with ASD might have difficulty feeling happiness, hopefulness, or joy.

What Is Post-Traumatic Stress Disorder (PTSD)?
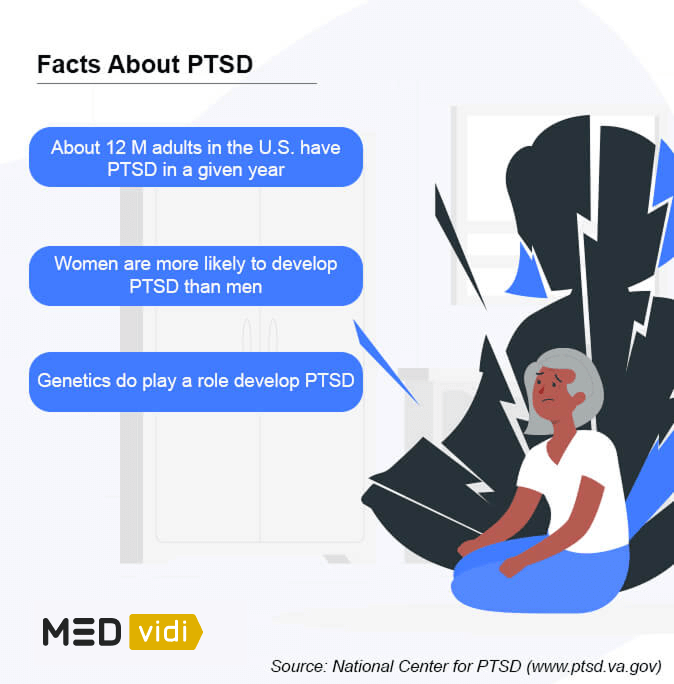
About
PTSD is a long-term mental health condition lasting more than a month, triggered by a traumatic event that affected the individual directly or indirectly. This causes ongoing distress and significant changes in thoughts and behavior, as well as poor function in more than one area of daily life. Communication issues and a sense of detachment may cause relationship issues; PTSD-related insomnia and anxiety can result in trouble concentrating, decreased productivity at work or academics, or absenteeism. Sometimes, it becomes difficult to perform daily routines and find pleasure in previously fulfilling activities.
Although PTSD can have similar symptom categories to ASD, negative changes in mood and thoughts are striking presentations in PTSD. Those with PTSD also tend to:
- have a bad outlook on themselves and everything around them;
- blame themselves and others for the trauma;
- no longer find enjoyment in life;
- constantly feel guilt, fear, shame, and sadness;
- are no longer able to experience joy, happiness, and contentment;
- may not remember the events and feel disconnected from others.
Symptoms of arousal, intrusion, and avoidance also occur and present very much like those for ASD described above; the dissociative symptoms might occur, but not as often as in ASD.
Key Differences Between ASD and PTSD
|
ASD |
PTSD |
|
|
Definition |
A short-lived mental health condition following a traumatic event |
A long-term mental health condition following a traumatic event |
|
Onset |
From 3 days after a trauma |
From at least one month after a trauma |
|
Duration |
Symptoms are present between 3 days and 4 weeks |
Persistence of symptoms for more than a month; can last for years |
|
Symptoms from most to least prominent |
|
|
|
Treatment |
|
|
|
Outcomes |
At least |
About |
Onset and Duration
The main distinguishing feature between ASD and PTSD is their timeline:
- An ASD diagnosis is made between 3 days and 1 month after the traumatic event.
- If symptoms are still present after (or for more than) a month, it suggests a PTSD diagnosis.
ASD lasts less than a month, while PTSD lasts months to years.
There can be a large time gap between the trauma and a PTSD diagnosis. In some cases, this might not happen until years after the event.
Common Symptoms
In ASD, the most common symptoms are dissociative, and the least prominent are negative mood symptoms; for PTSD, the opposite is true.
Treatment
ASD usually develops immediately after the trauma, so ‘psychological first aid’ by providing emotional and practical safety and support is essential.
Therapy is the first-line treatment for both disorders, but PTSD needs ongoing sessions for months or even years. Medication has not proved helpful in ASD, but might be prescribed ‘off-label’ if all else fails; however, certain antidepressants are authorized
Prognosis and Outcomes
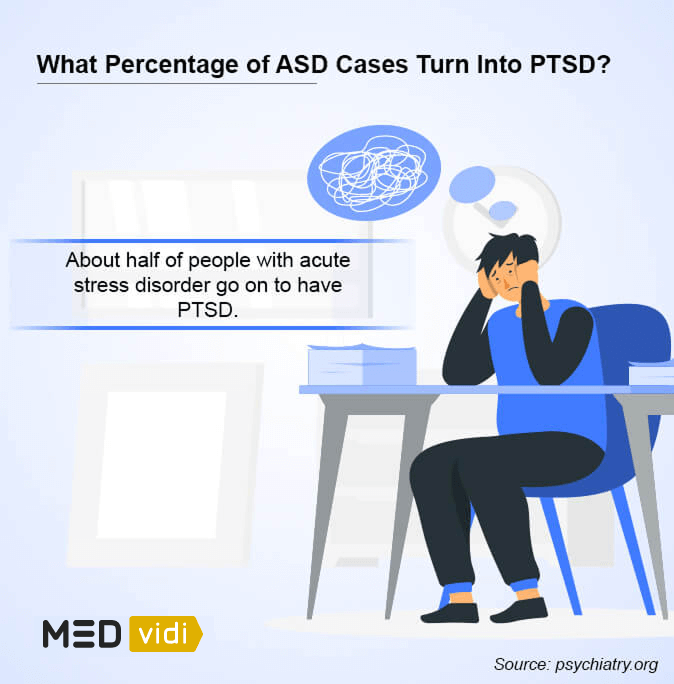
Although most people with ASD will recover from the condition with early treatment, having ASD results in a
If you’re experiencing suicidal or self-harming thoughts and require immediate assistance, contact a crisis hotline, such as 911, 988 suicide & crisis lifeline (toll-free), or Samaritans (116-123 or via chat).
Triggers and Risk Factors for ASD and PTSD
Potentially traumatic events that might lead to PTSD, and possibly ASD, might include:
- Sexual assaults
- Violent acts between people
- Natural disasters
- Serious accidents
- War or terrorism
- Extended physical or emotional neglect
- Interpersonal trauma (death or severe illness of a loved one)
However, people
So, other people at risk could be:
- Family or close friends of trauma victims
- First responders, e.g., police, firefighters, and ambulance personnel
- Doctors or nurses
- Therapists
Individual risk factors can also play a role in developing PTSD or ASD:
- A history of a mental health condition
- Previous trauma exposure
- Physical injury
- Lack of education
- Female gender
Younger age[7] - Poor socioeconomic status
- Poor access to support
- Extended hospital or
ICU stays[5] Severe pain[5]
Will Acute Stress Disorder Develop Into PTSD?
Between
Let’s discuss how doctors diagnose these disorders.
Diagnosis of ASD and PTSD
Mental health professionals need to follow strict diagnostic criteria or rules when confirming either ASD or PTSD; the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), written by the American Psychiatric Association, guides them.
Trauma-screening questionnaires also help to identify traumatic events in the patient’s history and PTSD symptoms, which are essential for the diagnosis of these trauma and stressor-related disorders. These can be self-reported checklists or structured questions asked by the doctor.
Treatment Options
Early interventions for any traumatic stress include creating a safe environment, providing emotional and practical support, and appropriate referral for treatment, which will vary depending on the event details and the individual’s risk factors. Let’s take a look at the options.
Evidence-Based Therapies
Cognitive Behavioral Therapy (CBT)
Cognitive behavioral therapy (CBT) focuses on changing inappropriate or unpleasant feelings associated with thoughts, which then changes behavior.
Specifically, trauma-focused CBT is the
- Educating people about trauma and its symptoms on the body and brain
- Teaching people how to manage these emotional and physical symptoms
- Identifying abnormal thought patterns, pointing them out, and challenging them
- Possibly introducing exposure therapy, another form of CBT
Exposure Therapy
Exposure therapy, as the name suggests,
Let’s say someone was in a serious car accident and now avoids driving or even being near cars. In exposure therapy, the person might gradually take the following steps:
- Look at pictures of cars
- Watch videos of cars driving
- Sit in a parked car
- Take a short drive
It can, unfortunately, make them feel worse in the beginning.
EMDR Therapy
Eye Movement Desensitization and Reprocessing (EMDR) therapy is a
In addition to psychotherapy, you may be recommended to maintain self-help routines. For example, regular physical activity, relaxation and grounding techniques, social interactions, and other personalized options.

Medication Options
Because ASD, by definition, is less than a month in duration, there is little evidence about the value of medication.
The antidepressants sertraline and paroxetine, which are selective serotonin reuptake inhibitors (SSRIs), are FDA-approved to treat PTSD. Sometimes, doctors use other SSRIs, selective serotonin and norepinephrine reuptake inhibitors (SNRIs), beta-blockers, antipsychotics, Prazosin, and Clonidine ‘off-label’ to help with symptoms.
When to Seek Help
If you have experienced a trauma and are having difficulty with your mental health, thinking of self-harm, or are having trouble functioning at work or home, it is essential to seek immediate help from a doctor or call a helpline. If this feels overwhelming, reach out to a loved one and ask them to help you book and be present with you at an appointment.
Conclusion
Both acute stress disorder (ASD) and post-traumatic stress disorder (PTSD) are triggered by traumatic events; however, their timelines define and distinguish them. Even though many of their triggers, risks, symptoms, and some treatment options overlap, significant differences might affect long-term outcomes.
This is why getting an accurate diagnosis from a mental healthcare professional is important. MEDvidi provides online appointments with experienced healthcare practitioners who will help diagnose ASD vs PTSD, and if appropriate, prescribe PTSD treatment. Book your appointment today.
Frequently Asked Questions About ASD and PTSD
Is PTSD similar to acute stress disorder, but more chronic?
The symptoms of PTSD and acute stress disorder (ASD) are similar, but while ASD lasts less than one month, PTSD symptoms are present for at least a month and can last years.
Can ASD turn into PTSD?
Yes,
How long does it take for acute stress disorder to become PTSD?
The development from acute stress disorder to PTSD happens after symptoms have been present for one month.
Can you have both ASD and PTSD at the same time?
No, you cannot have ASD and PTSD at the same time because of their distinct diagnostic criteria and timing differences.
What is the difference between PTSD and acute stress disorder and adjustment disorder?
PTSD and ASD require exposure to a traumatic event to cause specific diagnostic symptoms. Whereas, adjustment disorder requires emotional or behavioral symptoms out of proportion to an identifiable stressor, which could be moving house, getting divorced, or starting a new job.