Usually, depression is managed using medications or therapy, and for some patients, both options can be combined. Working closely with a psychiatrist will help to identify the most appropriate strategy for severe depression treatment.
However, sometimes, one can feel that their depression medication is not working. It is also possible that a patient may observe some brief improvement of symptoms only for them to turn worse and even more intense. Should this happen without any other explanation like a patient missing doses, then it is likely a case of treatment-resistant depression. In this post, let’s learn more about this condition and what can be done to overcome it.
If the symptoms of depression do not ease even though you follow all the doctor’s guidelines, you might have treatment-resistant depression. Consult with a therapist to know more.
What Is Treatment-Resistant Depression?
Presently, there is no unanimous definition for treatment-resistant depression (TRD). The agreed-upon guidelines for
It does not mean that one’s depression is untreatable. It will just require a different medication approach and more time. The prevalence of TRD is higher than one may have thought. According to studies (World Journal of Psychiatry, 2015), 30-40% of depression patients only experience partial remission of the symptoms, while 10% to 15% of depression patients do not see any improvement.
TRD significantly affects a patient’s health and should have urgent treatment and attention. It results in poor social functioning, increased mortality, and medical comorbidity. Untreated depression can increase one’s lifetime suicide risk
Main Symptoms of TRD
Treatment-resistant depression may
- Lack of positive response after psychotherapy or medication treatment.
- Lacking adequate response after standard depression treatment.
- Small or temporal improvements which are followed by a return of depressive symptoms.
- More frequent, longer, and more severe depression episodes.
- Increased anxiety.
- Extended changes in appetite where a patient is skipping meals and lacks appetite, even for dishes they usually like.
- Disruptive sleep patterns, especially waking early in the morning, and a patient cannot go back to sleep.
- Constant suicidal and self-harm thoughts.
On top of these symptoms, patients should seek expert help if the side effects of the medications have been too severe to handle or if they have observed some improvement, but they are not fully back to their old selves.
Have you noticed some of the above symptoms? MEDvidi professionals will provide the best treatment for depression.
Causes of Treatment-Refractory Depression
The exact causes of treatment-refractory depression are unknown, but experts believe the following factors have a significant contribution.
1. Misdiagnosis
A wrong diagnosis can result in a poor response to depression medication. For example, one could have the symptoms of major depressive disorder and bipolar disorder. If the doctor prescribes standard medications for MDD, it will not be effective as it will not address the bipolar condition.
2. Genetics
According to
3. Metabolic Disorders
Patients’ metabolism may also affect how they process their medication. Certain nutritional deficiencies have also been associated with treatment-resistant depression. According to
Other factors can increase a person’s risk of having TRD. These include:
- Patients who have had major depression for a long period or their depression episodes last longer.
- Patients with severe and mild depression symptoms may not respond well to antidepressants.
- Patients with other conditions along with depression, for example, anxiety, have a high risk of having depression that is resistant to treatment.
- Patients whose depression onset started at an early age.
- Patients with depression who are older.
Depression can develop in anyone, the range of its causes is very wide. Don’t hesitate to seek help if you feel unwell.
Treatment for Resistant Depression
There are three approaches to
- Medication management.
- Psychological counseling.
- Medical procedures.
Medication Management
Some of the options a psychiatrist may recommend include:
- Pharmacogenetic testing. These tests evaluate specific genes providing insight into how your body will process varied medications. They may help identify effective drugs and ones with tolerable side effects.
- Increasing the dosage of current medicine. Different people respond to antidepressants differently, and in some cases, a higher dosage may prove effective.
- Using off-label medication. The doctor may also use off-label medications for treatment-resistant depression and an antidepressant. This strategy is called augmentation, and some of the medications used include anti-anxiety drugs, antipsychotics, stimulants, thyroid hormone drugs, and mood stabilizers.
- Changing antidepressants. The doctor may also switch a patient’s antidepressant since, for some patients, the first anti-depressant is often not effective.
- Adding a different kind of antidepressant. The doctor can also consider using two different classes of antidepressants simultaneously. This strategy targets neurotransmitters affecting mood, including serotonin, norepinephrine, and dopamine.
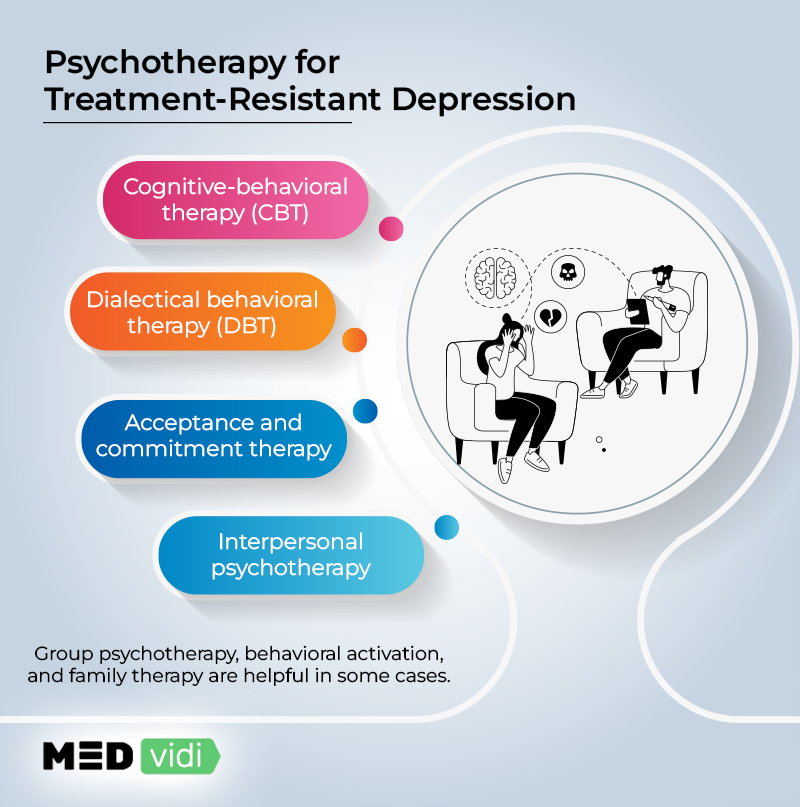
Psychotherapy
Psychological counseling by a mental health expert can be very effective, especially when used along with medication. It has lasting effects as it helps identify underlying issues behind the depression and provides better behaviors for coping. Different approaches should be tried or combined to identify the most effective option. Some of them include:
- Cognitive-behavioral therapy
- Interpersonal psychotherapy
- Dialectical behavioral therapy
- Group psychotherapy
- Behavioral activation
- Family/marital therapy
- Commitment and acceptance therapy
Medical Procedures
Where psychotherapy and medications are not working, the following alternative treatment procedures may be considered.
- Repetitive transcranial magnetic stimulation (RTMS). In
this procedure[7] , magnetic fields are used to stimulate nerve cells to relieve depression symptoms. It targets nerve cells in the brain region, controlling mood and depression. It is usually done across 30-minute sessions through rapid bursts. - Ketamine therapy. Ketamine is a medication usually given through IV line to provide fast relief from treatment-resistant depression symptoms. It is usually administered in low doses, with its effects lasting up to weeks. There is an FDA-approved intranasal version called Esketamine for adults given under the supervision of a health care provider who monitors potential severe side effects, misuse, or abuse.
- Electroconvulsive therapy (ECT). In this procedure, a measured electricity dose is passed through one’s brain while asleep, intentionally triggering a small and short-lasting seizure. It causes changes in the brain’s chemical state and can quickly reverse symptoms of severe depression.
- Vagus Nerve Stimulation (VNS). This therapy is the last resort after all the above procedures have proven unsuccessful. It uses an implanted device in the chest connected to the vagus nerve in the neck to send signals to the brain mood centers, which helps improve depression symptoms.
Conclusion
All these options are available for patients with treatment-resistant depression. As such, there is no need to lose hope. It is vital that patients work closely with their doctors to provide regular feedback on their recovery progress. They should also not hesitate to change their physicians if they feel they need expert help on how to deal with treatment-resistant depression.













