Highlights
- Mood disorders are mental health conditions characterized by striking disturbances of mood and motivation.
- The mood changes seen in mood disorders can be severe lows (depressive episodes) or severe highs (manic episodes).
- There are two broad types of mood disorders, depressive and bipolar and related disorders, each having subtypes.
Mood, be it sadness, happiness, contentment, or irritability, influences your behavior. And during the course of a day, it is entirely normal to have mild mood swings depending on what’s happening around you. But ‘mood disorder’ implies a problem, so when do changes in feelings become an issue?
This article will examine examples of mood disorders, their symptoms, diagnosis, and treatment.
Feeling low or emotionally unstable for a while? See a licensed healthcare provider for an online mental health assessment.
What Are Mood (Affective) Disorders?
The definition of a mood disorder includes a striking mood disturbance or instability, which can either be an extreme low (called depression) or a severe high (called mania).
The term ‘affective disorders’ is an older term for mood disorders, which some doctors may still use.
When we talk about types of mood disorders, it’s usually the two umbrella categories: depressive and bipolar and related disorders. They are defined and diagnosed using the two main symptom groups: depressive and manic episodes.
Symptoms of Mood Disorders
Let’s chat about these depressive and manic mood symptoms before we tackle the disorders themselves. We’ll look at changes in emotions and thinking, as well as physical signs and symptoms.
Depressive Episodes
Extreme or inappropriate emotional presentations:
- Sadness
- Emptiness
- Hopelessness
- Irritability
- Experiencing no interest or pleasure
Changes in thinking:
- Poor concentration
- Poor memory
- Negative thoughts, for example, “I’m worthless,” or “What’s the point of life?”
- Brain fog
Physical manifestations:
- Exhaustion
- Sleeping too much or too little
- Eating more or less than usual
- Aches and pains, for example, headaches or stomach issues

Manic (or Hypomanic) Episodes
| Manic Episode | Hypomanic Episode |
OR
OR
|
|
|
|
The person having the manic episode
Shared Symptoms in Both Hypomania and Mania
Extreme or inappropriate emotional presentations:
- Cheerfulness
- Optimism
- High energy
- Confidence
- Friendliness
- Irritability
- Extreme mood swings and anger
Changes in thinking:
- Racing thoughts
- High distractibility
Physical manifestations:
- Increased talkativeness
- Rapid speech
- A decreased need for sleep
- Restlessness, like pacing or tapping
- Increased impulsiveness
- Over-working
Commonly Seen in Manic Episodes
Changes in thinking can also involve psychotic features:
- Delusions: Believing things that aren’t real.
- Hallucinations: Seeing, hearing, or smelling things that aren’t real.
- Grandiosity: An exaggerated sense of one’s own importance, abilities, or power. It is not usual self-confidence. Examples may be believing that they:
- Don’t need to study because they’re more intelligent than the professors.
- Can start multiple businesses with no plan or finances.
- Can claim they can heal people with their minds.
Types of Mood Disorders
Below is a list of the different mood disorders, providing you with a clear picture, before we discuss them in detail.
1. Depressive Mood Disorder Types (the more common mood disorders)
- Major depressive disorder (MDD)
- Persistent depressive disorder or dysthymia (PDD)
- Premenstrual dysphoric disorder (PMDD)
- Disruptive mood dysregulation disorder (DMDD)
- Seasonal affective disorder (SAD)
- Substance/medication-induced depressive disorder
- Depressive disorder due to another medical condition
- Unspecified depressive disorder
2. Bipolar Mood Disorder Types
- Bipolar I disorder
- Bipolar II disorder
- Cyclothymic disorder
- Substance/medication-induced bipolar disorder
- Bipolar disorder due to another medical condition
- Unspecified bipolar disorders
3. Unspecified Mood (Affective) Disorder
Depressive Disorders
Major Depressive Disorder (MDD)
Often considered the most common mood disorder, MDD is diagnosed when at least five out of the nine symptoms listed below are present for at least 2 weeks and cause poor functioning in daily life.
- Sad mood
- Insomnia
- Feelings of guilt
- Low energy levels
- Poor concentration
- Poor or increased appetite
- Finding no enjoyment or pleasure in things that were pleasant before
- Being restless or sluggish
- Recurrent self-harm or suicidal thoughts or acts
A few facts about depression:
- Major depressive disorder is the most common type of mood disorder in both men and women. But
women are twice[2] as likely to have MDD during their lifetime compared to men. - The lifetime prevalence of MDD is approximately
5-15%[2] . - In a year, about
7 out of 100 U.S. adults[2] will have depression. - Depression is one of the leading causes of disability worldwide.
Persistent Depressive Disorder (PDD or Dysthymia)
Premenstrual Dysphoric Disorder (PMDD)
This mood disorder affects females, usually starting a week before menstruation and lasting three to seven days after the first day. Rapid mood swings are a hallmark feature of this condition, as are depressive mood, anxiety, and physical symptoms.
Seasonal Affective Disorder (SAD)
Depressive episodes
Disruptive Mood Dysregulation Disorder (DMDD)
It is a new diagnosis that appeared first in the DSM-5-TR and only affects children and adolescents. People with DMDD have
Other Specified and Unspecified Depressive Disorders
These are depressive episodes that don’t fit into the conditions discussed above.
If you’re experiencing suicidal or self-harming thoughts and require immediate assistance, contact a crisis hotline, such as 911, 988 suicide & crisis lifeline (toll-free), or Samaritans (116-123 or via chat).
Bipolar Disorders (BD)
Bipolar I
Bipolar I is diagnosed if the person with the mood disorder has
Bipolar II
Bipolar II is diagnosed if the person with the mood disorder has

Cyclothymia
Cyclothymia is a tricky one; essentially, it consists of
Other Specified and Unspecified Bipolar Disorders
These are presentations that don’t fit into the bipolar-type conditions discussed above.
A few facts about bipolar disorder:
- Men and women are usually
equally affected[6] by bipolar disorders. - In a year, about
3 out of 100 U.S. adults[2] will be diagnosed with bipolar disorder. - The lifetime prevalence of bipolar disorder is about
4%[3] .
In
Unspecified Mood Disorder
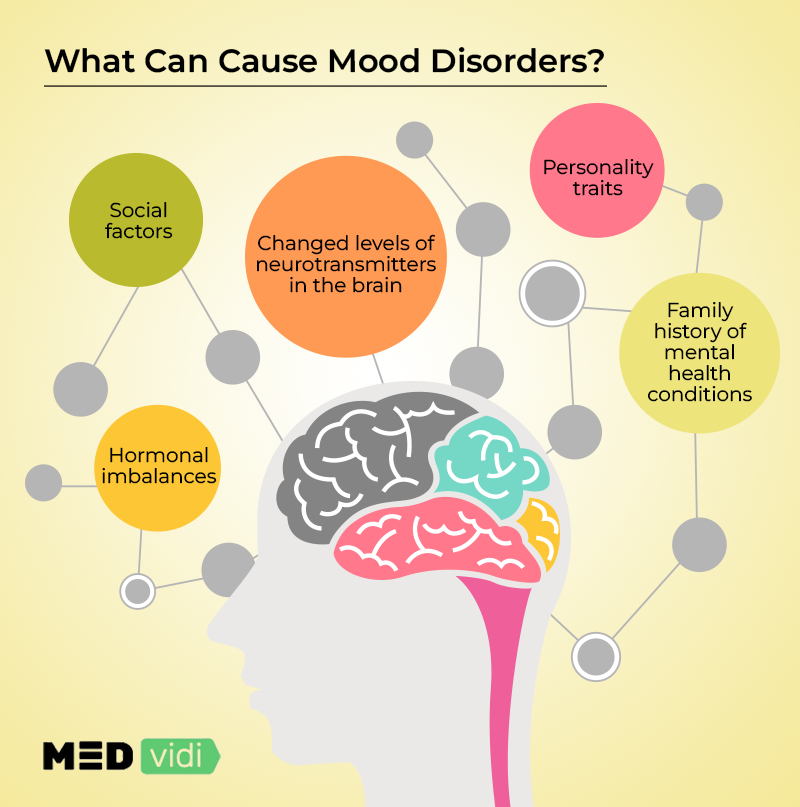
Risk Factors and Causes of Mood Disorders
The exact
Brain Chemistry Factors
Certain neurotransmitters, including serotonin, norepinephrine, and dopamine, play a crucial role in regulating mood.
Genetic Factors
A positive family history of mood disorders is a substantial risk factor. So, children and siblings of people with mood disorders are more likely to be diagnosed with the condition themselves.
Social Factors
Medical Conditions and Medication
Medical Conditions
A long-term illness, for example, cancer, severe arthritis, or lung problems, can cause depressive symptoms in patients because they are no longer able to do what they used to. Also, certain medical conditions can directly trigger mood disorders; some examples of these include vitamin B12 and D deficiencies, HIV, syphilis, brain tumors, and multiple sclerosis (MS).
Hormonal imbalance can also cause physical and psychological problems. For example,
Medications
Sometimes, medication or illicit drugs can trigger depressive or manic episodes; your healthcare provider will consider this when reviewing your history. A few examples are steroids, birth control pills, blood pressure medication, epilepsy medication, alcohol, drugs of abuse, sleeping tablets, and even certain antibiotics.
Other Conditions Commonly Diagnosed with Mood Disorders
Often, other mental health conditions coexist with mood disorders. Here are a few examples:
- Generalized anxiety disorder
- Panic disorder
- Obsessive-compulsive disorder (OCD)
- Post-traumatic stress disorder (PTSD)
- Attention-deficit hyperactivity disorder (ADHD)
- Borderline personality disorder (BPD)
- Schizophrenia
Co-occurring conditions can complicate matters for a few reasons:
- Sometimes, the symptoms overlap, making diagnosis tricky.
- When there are multiple mental health conditions, finding a treatment to cover all the symptoms is often difficult, making the road to recovery longer.
Diagnostic Process for Mood Disorders
- Booking a Consultation. The first step to getting a mood disorder diagnosis is to make an appointment with a healthcare professional and have an assessment.
- Chatting Through Your Symptoms. A healthcare provider will listen to your story and ask specific questions about symptoms that point towards manic and depressive episodes. They may also use specific mood disorder questionnaires to aid in the diagnosis.
- Taking Health History. They will take a family history and ask about your current and past medications and medical conditions.
- Having an Examination and Investigations. If the healthcare professional suspects another medical condition is the cause, they may refer you for special investigations, such as brain scans or blood tests, to rule it out.
- Making the Diagnosis. With all this information, they will use the Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR) to decide:
- If there is a mood disorder present
- What type and subtype is it
Once this is confirmed, a healthcare provider will decide on appropriate treatment options.
Mood Disorder Treatment
Treatments for mood disorders usually include medications and mental health therapies.
Medications
There are three main classes of medications used to treat mood disorders.
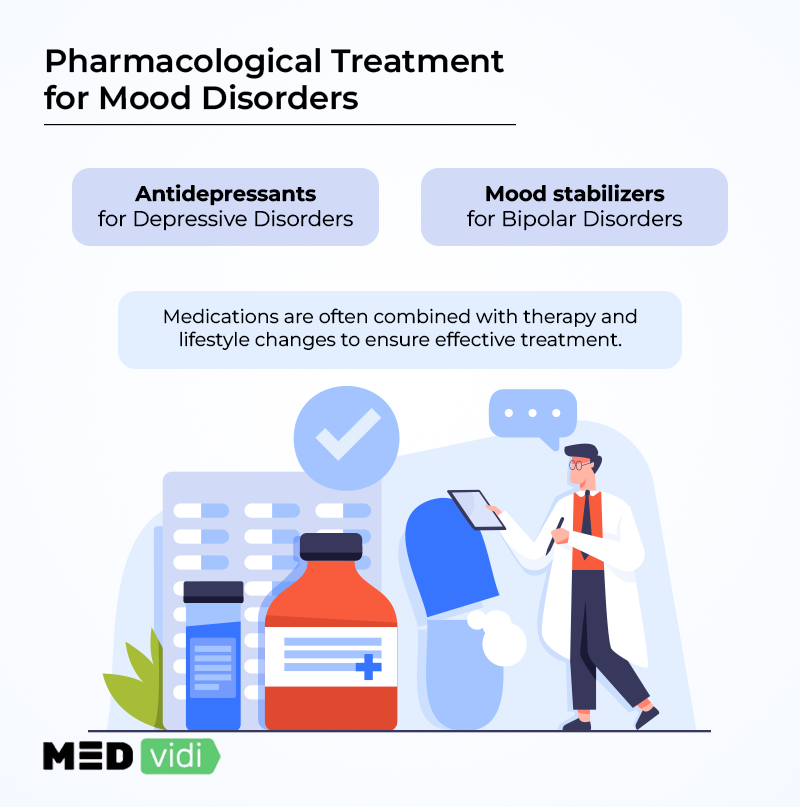
Antidepressants
Antidepressant medications mainly treat depressive disorders, although occasionally they are used for the depressive episodes seen in bipolar disorders in combination with mood stabilizers.
SSRIs (selective serotonin reuptake inhibitors) and SNRIs (serotonin-norepinephrine reuptake inhibitors) are the most commonly prescribed antidepressants due to their better safety profile and tolerability. It usually takes them 4 to 6 weeks to start working.
Mood Stabilizers
Mood stabilizers help to prevent severe mood swings and manic episodes; they are often
Antipsychotics
Antipsychotics are
Mental Health Therapy
Different psychotherapies are helpful to treat mood disorders; the more common ones include:
Cognitive-Behavioral Therapy (CBT)
CBT is the most widely used therapy for mood disorders. It helps patients identify and change thoughts that are affecting their moods, allowing them to modify their behavior.
Interpersonal Therapy
This therapy focuses on the fact that
Family Therapy
Firstly, this type of therapy helps patients understand how their condition impacts their family. Secondly, it educates family members about the condition, helping them to be more tolerant and supportive. And finally, if the condition’s trigger was a family stress, therapy can help resolve the situation.
Psychoanalytical Therapy
Less Common Treatment Options
There are some additional treatment methods sometimes used for severe forms of mood disorders; they include:
Electroconvulsive Therapy (ECT)
ECT involves passing electrical currents through electrodes into the brain, inducing a mild seizure. Usually, it is used because the medications available haven’t helped.
Vagus Nerve Stimulation (VNS)
Electrical impulses stimulate the vagus nerve to regulate mood symptoms, and it is
Transcranial Magnetic Stimulation
It involves sending short bursts of magnetic energy to the targeted brain regions to manage mood disorders and is
Light Therapy
People with SAD (seasonal affective disorder) are exposed to light that mimics natural sunlight.
Lifestyle Changes
Making small adjustments in daily life activities may speed up the recovery process.
Regular Exercise
Physical exercise boosts physical and mental health, justifying the proverb, ”A healthy mind in a healthy body.” It doesn’t have to be strenuous exercise; a daily 20-30 minute walk can also be effective if done consistently.
Balanced Diet
Cutting back on junk food and switching to organic foods, such as vegetables, whole grains, and white meat, can have a profoundly positive impact on mental health.
Yoga and Other Relaxation Techniques
Yoga, mindfulness, breathing exercises, and meditation are effective for lowering stress levels and boosting happy chemicals in the brain.
Avoiding Smoking, Vaping, and Alcohol Consumption
Smoking or vaping and alcohol consumption can make a person feel depressed and anxious when the alcohol and nicotine levels drop. Alcohol consumption should be cut down to less than 2 units per day for men, and 1 unit per day for women, although even small amounts carry health risks.

Outlook and Prognosis
Unfortunately, there is no way to predict whether treatment will be effective, how long it will take to control symptoms, or how long the remission will last. This is because not everyone’s body or mood disorder presentation is identical. However, there are a few trends:
- About 5 to 10 percent of the patients with MDD eventually
develop bipolar disorder[9] . MDD often recurs[9] , with the likelihood of a future relapse increasing with every episode. This is why ongoing management is important.
People with mood disorders
- More than one mental health condition
- A personality disorder
- Multiple hospitalizations
- A mood disorder diagnosed later in life
On the other hand, they have a
- Mild symptoms
- No psychotic features, including delusions or hallucinations
- Been taking their medication correctly and long-term
- Regular follow-ups with their mental health professionals
When to Seek Help
Early diagnosis and treatment improve the outcome, so if you think that you might have a mood disorder and are experiencing any of the following ‘mood disorder warnings’, seek help as soon as possible:
- Your extreme low or high moods are affecting relationships and functioning at home or work.
- You are using alcohol or illicit drugs.
- You are seeing or hearing things that no one else does.
- You believe something is true, even though there is clear evidence it isn’t
- You are thinking about self-harm or suicide.
- You are thinking about harming someone else.
At MEDvidi, you can see a licensed healthcare provider who will start the process by conducting an accurate online mental health assessment and making a diagnosis. Should this be a major depressive disorder, they will create a customized treatment plan and continue to monitor the progress throughout the recovery phase. For bipolar and related disorders, MEDvidi’s team can make a diagnosis and recommend next steps, helping to get you to the appropriate mental health professionals.
Book an appointment and experience high-level care from the comfort of your home.
Mood Disorders FAQs
How are mood disorders diagnosed?
Doctors diagnose mood disorders by carefully assessing symptoms through questionnaires and health history review, ruling out other possible medical causes, and ensuring that the DSM-5-TR criteria are met.
Are mood disorders similar to personality disorders?
Mood disorders and personality disorders are not similar, although they are both recognized mental health conditions; their course and predominant symptoms differ. Mood disorders primarily affect emotions, whereas personality disorders directly disrupt behavior and thinking patterns.
How common are mood disorders?
According to statistics, an estimated 9.7% of US adults are likely to be diagnosed with a mood disorder in any given year. The ratio is higher for females than for males.
Is anxiety considered a mood disorder?
No, anxiety is not considered a mood disorder. However, an uncontrolled lifelong anxiety disorder might trigger a mood disorder if a person’s anxiety is affecting their daily functioning, making them feel extreme sadness.
Are mood disorders lifelong?
Mood disorder episodes often recur and may be lifelong. The likelihood of a future relapse increases with every new episode, so it is important to get a diagnosis early, take treatment correctly, and follow up regularly.
Is mood disorder considered a disability?
If a severe mood disorder interferes with the patient’s daily life to the extent that they cannot function at all, then it might qualify as a disability. It may also entitle patients to apply for Social Security Disability (SSD) benefits.
Can untreated ADHD cause mood disorders?
Yes, untreated ADHD can increase stress and anxiety levels that may ultimately lead to the development of a mood disorder.
What are the 5 mood disorders?
There are two broad groups of mood disorders, the depressive and bipolar types. The depressive group includes: major depressive disorder (MDD), persistent depressive disorder or dysthymia (PDD), premenstrual dysphoric disorder (PMDD), disruptive mood dysregulation disorder (DMDD), and seasonal affective disorder (SAD). The bipolar group includes: bipolar I disorder, bipolar II disorder, and cyclothymic disorder, among others.
What is the most common mood disorder?
The most common mood disorder is major depressive disorder, which affects seven out of every 100 adults in the US.
What is the rarest mood disorder?
Cyclothymia is often considered the rarest mood disorder according to statistics; however, there is limited data about the unspecified type and subtypes.
What is the hardest mood disorder to live with?
There isn’t one specific mood disorder that is hardest to live with, as every individual’s situation is different. The outcome depends on a few factors, including the severity of the symptoms and the availability of support systems and treatment options.
What triggers mood disorders?
Mood disorders are usually influenced by multiple factors, for example, a family history, stressful life events, an abusive childhood, certain medical conditions, medications, and substance abuse.
What are disorders similar to bipolar disorder?
Mental health conditions that might present with similar symptoms to bipolar disorders include: borderline personality disorder, and schizoaffective disorder.
How does a mood disorder affect daily life?
A mood disorder can impact relationships and the person’s ability to perform routine chores and work tasks, due to changes in thinking, energy levels, and motivation.
Is depression a mood disorder?
Yes, major depressive disorder is a mood disorder; one of its depressive episodes could indicate MDD alone, or form part of a bipolar diagnosis, if the person has also experienced manic episodes.